Tylenol and Fetal Autism Risk: Transparency, Science, and the Pushback from Medical Establishment
In a bold move this September 2025, the U.S. Food and Drug Administration (FDA) announced it was initiating a label change for acetaminophen—commonly known as Tylenol—to include warnings about potential risks of autism spectrum disorder (ASD) linked to its use during pregnancy.
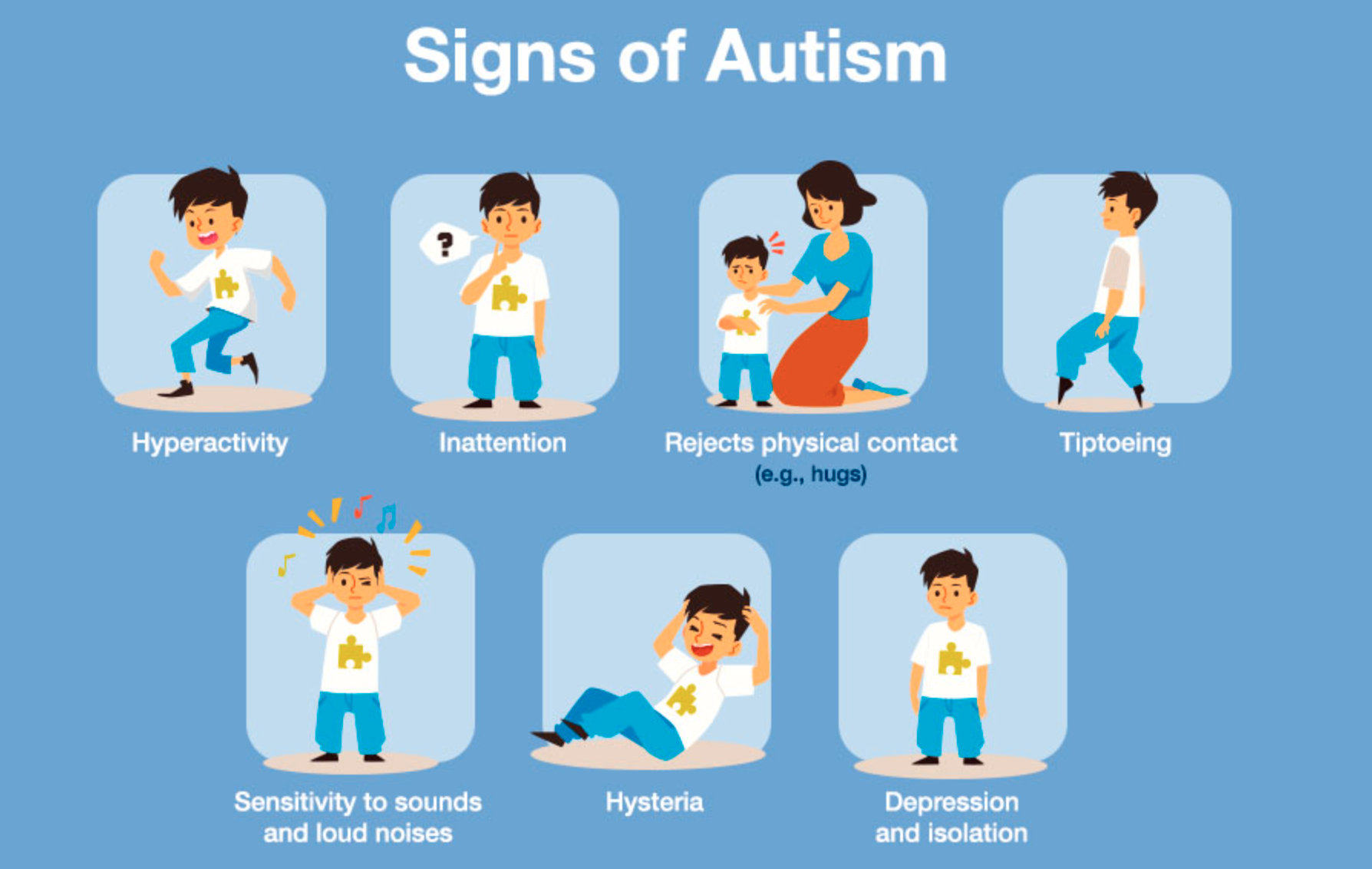
This comes amid growing evidence from studies suggesting prenatal exposure to the drug may elevate the risk of neurodevelopmental issues in children, including autism and ADHD.
Echoing historical tragedies like thalidomide, which caused severe birth defects in the 1950s and 60s (see this survivor's story), the announcement highlights the need for caution with medications during pregnancy. Don't panic, though—Tylenol remains widely available over-the-counter (OTC) without a prescription, and its price hasn't changed. The FDA's action isn't a ban; it's about bringing hidden information into the light, information that pharmaceutical companies and medical groups may have downplayed.
Medicine is an evolving field, and raising questions about potential problems is essential for progress. If you shy away from these discussions, you're essentially dismissing the value of free speech in science. The Science Behind the Link: Glutathione Depletion and Fetal DevelopmentAcetaminophen works by being metabolized in the liver, where it binds to glutathione—a critical antioxidant that's not just "nice to have" but essential for survival. Depleting glutathione can lead to oxidative stress, which is particularly harmful during pregnancy.
In cases of overdose, the antidote is N-acetylcysteine (NAC), which replenishes glutathione, underscoring how the drug directly impacts this pathway. Prenatal glutathione depletion from acetaminophen has been associated with:
Fetal developmental delays
Neural system abnormalities
Increased risks of pregnancy complications like preeclampsia
Studies show that acetaminophen exposure may disrupt neurodevelopment through oxidative stress and endocrine pathways, potentially leading to reproductive, hepatic, and behavioral issues in offspring.
Animal models and human data suggest it can cause neurodevelopmental injury in susceptible fetuses.
A quick PubMed search reveals numerous papers exploring the acetaminophen-autism connection. Here are some key ones from the original discussion, plus additional recent research:
More recent studies bolster this:
A 2024 JAMA analysis found marginally increased risks of autism with prenatal exposure, though sibling controls tempered the association.
Mount Sinai's 2025 study linked it to higher autism and ADHD risks.
Harvard research from 2025 suggests prolonged use correlates with elevated neurodevelopmental risks.
A PMC review highlights acetaminophen's role in potential neurobehavioral dysfunctions.
Environmental Health Perspectives evaluated evidence showing over 50% of pregnant women use it, with calls for more research.
It's not that every Tylenol dose causes autism—it's about increased risk through pathways like inflammation and oxidative stress.
The Vaccine Connection: A Compounding Risk? Fever after vaccinations is common, and Tylenol is often recommended to manage it. However, vaccines can introduce elements that accumulate (like aluminum adjuvants), and combining this with acetaminophen's glutathione depletion may exacerbate brain inflammation, damaging neural cells and potentially contributing to autism.
This oxidative stress-inflammation nexus is a recurring theme in autism research.
Informed doctors have long cautioned against routine post-vaccine Tylenol use. Why the Backlash? Cognitive Dissonance in Medicine Medical organizations like ACOG and SMFM have pushed back, affirming acetaminophen's safety based on current data.
Even the WHO states no conclusive link exists.
This resistance may stem from years of recommending the drug to pregnant women and infants alongside vaccines, creating cognitive dissonance. Ignoring or downplaying emerging evidence doesn't serve patients—doctors treating mothers and children should be aware and cautious. As science advances, embracing tough questions is key. The FDA's transparency is a step forward, reminding us that what was once "safe" can face scrutiny. Stay informed, discuss with your healthcare provider, and prioritize evidence-based choices for you and your family.