In the world of hormones that influence our health and weight, leptin stands out as a crucial player. Discovered relatively recently, this hormone has garnered significant attention in functional medicine and health discussions. If you're familiar with topics like insulin resistance or metabolic health, you've likely encountered leptin before. In this article, we'll dive deep into what leptin is, how it functions, its role in weight control, the common issue of leptin resistance, and practical steps to manage it effectively.
Leptin is often described as an "appetite-suppressing" hormone, and for good reason—it acts as an ally in preventing excessive weight gain. Produced primarily by fat cells (adipocytes), leptin helps regulate body weight by influencing two main processes: reducing appetite to limit food intake and increasing energy expenditure to burn more calories.
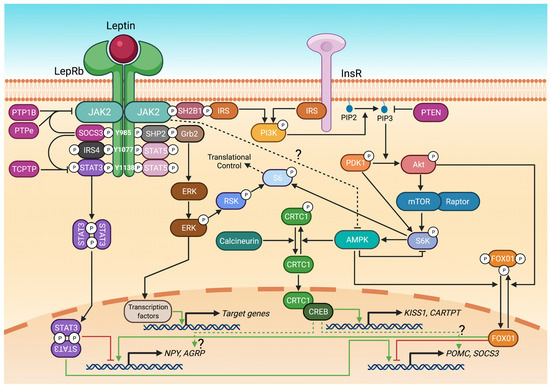
At its core, leptin functions as a signaling molecule. Hormones, in general, are chemical messengers that travel through the bloodstream to communicate between organs, tissues, or the brain. Leptin specifically carries messages from fat cells to the brain, informing it about the body's energy status. It essentially reports: "How much fat is stored? Is there surplus energy, or do we need more?"
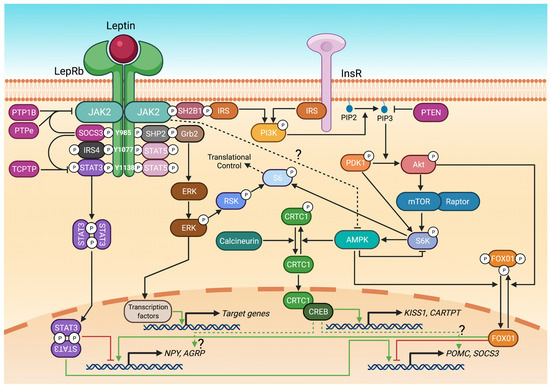
In a healthy, well-functioning body, this system works seamlessly. When fat accumulation increases—indicating ample energy reserves—fat cells release more leptin. This signal reaches the brain's hypothalamus, which interprets it as a cue to curb hunger and prevent further fat storage. The result? You feel less inclined to overeat, and your metabolism stays efficient.
This might seem counterintuitive: Why would fat cells produce a hormone that limits their own growth? Think of it as a built-in feedback loop designed to maintain balance. Leptin ensures the body doesn't hoard unnecessary fat, promoting overall energy homeostasis.
Unfortunately, this ideal scenario doesn't always hold in modern life. Many people develop leptin resistance, a condition strikingly similar to insulin resistance. In leptin resistance, fat cells continue to produce and send leptin signals, but the brain fails to respond properly. It's not that the brain is deliberately ignoring the message; rather, chronic overexposure to high leptin levels desensitizes the receptors, making the signals ineffective.

What causes this resistance? The primary culprit is excess body fat. When fat cells are overloaded, they secrete abnormally high amounts of leptin. Over time, this constant barrage leads to a breakdown in communication. From the brain's perspective, it's as if no signal is arriving at all.
To illustrate, imagine an ancient kingdom where fat cells are like ministers reporting to the king (the brain). The ministers send petitions (leptin) about the "village" (body fat) being overstocked with resources. But if these petitions get lost or ignored, the king assumes the village is starving. In response, the king orders austerity measures: conserve energy, ramp up food collection, and store every bit of surplus for famine. Translated to the body, this means:
The outcome? A vicious cycle where weight gain accelerates, despite the body's original intent to maintain balance. This miscommunication turns leptin from an ally into a silent saboteur.
Just as addressing insulin resistance is vital for metabolic health, tackling leptin resistance is key to sustainable weight loss. The good news? These issues often resolve together. Strategies that improve insulin sensitivity—such as better diet and lifestyle habits—also help restore leptin signaling. It's a "two-for-one" effect: fix one, and the other follows.
Early research on leptin was promising. Scientists hoped injecting or administering leptin could revolutionize dieting by directly suppressing appetite. However, experiments showed little to no effect, and high doses often worsened resistance, much like overusing insulin in diabetes management. This underscores a critical lesson: hormones aren't just about quantity; effective signaling is what matters. Simply boosting levels without addressing resistance leads to poor outcomes.
Leptin levels can be measured through blood tests, with a normal range typically below 12 ng/mL. Balance is crucial—deviations in either direction spell trouble:

Factors that elevate leptin include sleep deprivation, chronic stress, and thyroid dysfunction. Leptin interacts closely with stress hormones like cortisol, and it's common in people with insulin issues or hypothyroidism.
Leptin resistance doesn't exist in isolation; it's often intertwined with other hormonal imbalances, particularly thyroid function. Hypothyroidism—low thyroid activity—is notorious for causing weight gain. Even subclinical (functional) hypothyroidism, which may not show up on standard tests, can contribute.
High leptin levels interfere with thyroid hormone conversion. The thyroid produces T4 (thyroxine), which must convert to the active form T3 (triiodothyronine) to regulate metabolism. Elevated leptin reduces this conversion, increasing "reverse T3" (an inactive form) and making weight loss harder. Patients on levothyroxine (synthetic T4) may find it less effective if leptin is high, leading to frequent dose adjustments.
If you're struggling with unexplained weight gain, consider testing leptin alongside thyroid markers. Adding iodine (under medical guidance) can support T4-to-T3 conversion and enhance treatment efficacy, as supported by research.
The path to resolving leptin and insulin resistance starts with lifestyle changes. Since these conditions stem from modern dietary and habitual pitfalls, targeted adjustments can restore balance:

If these concepts feel overwhelming, think of them as interconnected puzzle pieces. Exploring related topics like insulin resistance, metabolic syndrome, and thyroid health can provide deeper insights—many resources, including books and educational videos, tie them together.
Leptin is more than just a weight-control hormone; it's a vital messenger in your body's energy regulation system. When functioning well, it keeps appetite in check and prevents excess fat storage. But in the face of resistance—driven by poor diet, stress, and other factors—it can lead to weight struggles, metabolic issues, and broader health risks. The empowering news is that you can influence leptin through everyday choices, often resolving it alongside insulin resistance for amplified benefits.
If persistent weight issues or related symptoms persist, consult a healthcare provider for testing and personalized advice. Small, consistent changes can realign your hormones and transform your health. Stay informed, and take proactive steps toward balance.
```