
By Dr. Cho
Hello, everyone! As a physician passionate about empowering patients, I've seen firsthand how prevalent high blood pressure has become. In recent years, the number of people managing this condition with medications has skyrocketed, showing no signs of decline. But what exactly is high blood pressure, and more crucially, why do so many of us develop it? In this article, we'll explore these questions, debunk common myths, and emphasize why understanding your condition is key to potentially reducing or even eliminating reliance on lifelong medications.

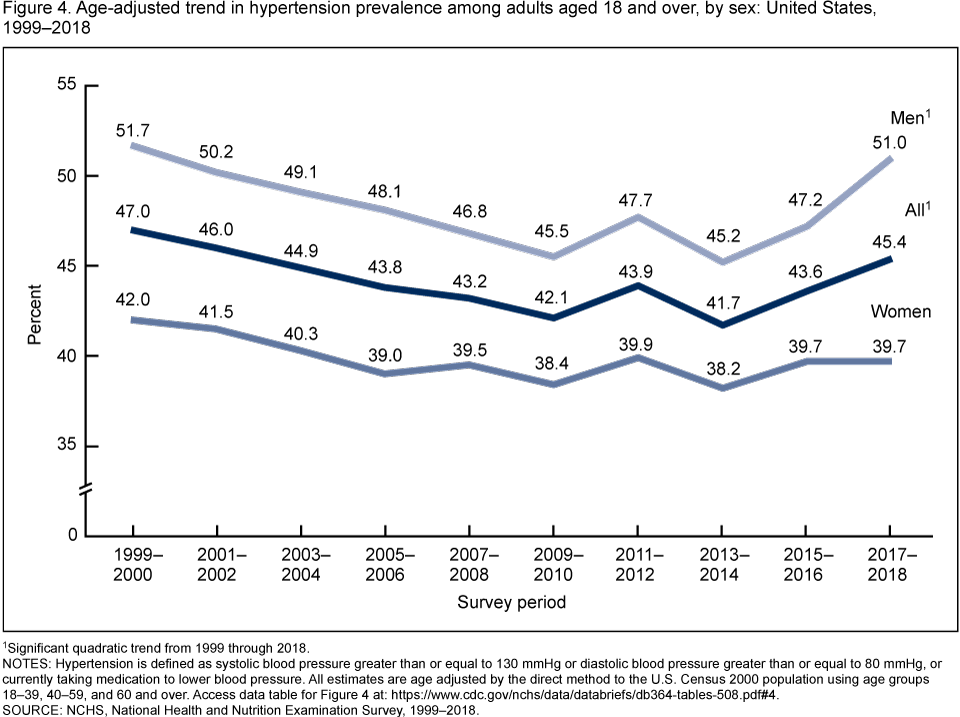
High blood pressure, or hypertension, affects millions worldwide. In the United States alone, over 100 million adults—about one-third of the population, or nearly half when excluding children—live with it. Globally, the figure approaches one billion, with more than half of cases accompanied by diabetes and 40% involving both diabetes and high cholesterol. Many patients I speak with can't explain why they've developed hypertension. Some even shrug it off, thinking, "Isn't that the doctor's responsibility?" While it's true that for acute emergencies—like severe injuries, unconscious states, or specialized surgeries—we fully entrust experts, chronic conditions are different. Hypertension, diabetes, and high cholesterol often require ongoing clinic visits for prescriptions, but they're managed at home without hospitalization. This means you play a central role in your care. These illnesses frequently stem from lifestyle factors we've contributed to, so taking an active interest is essential for improvement. By understanding and addressing root causes, true healing becomes possible. This might even mean weaning off medications. Pills are a temporary fix for acute spikes in blood pressure or sugar levels—to "put out the fire." Once stabilized, investigate the underlying issues. Resigning to lifelong medication? At least be informed about the downsides. Blood pressure drugs can lead to side effects like acid reflux, gastrointestinal problems, joint pain, muscle aches, or accelerated dementia. Weigh these risks against benefits before committing. Sadly, many remain unaware, attributing new symptoms—like heartburn or leg cramps—to "just getting old." They end up on additional meds, compounding the issue. When we discuss "quitting meds," it's not about rejecting them outright but dispelling the myth that they're an unbreakable shield. Aim for independence from them where possible. I'm not anti-medication—far from it. We're thankful for tools like painkillers and antibiotics. But overuse is harmful, and the same applies here: treating hypertension or diabetes drugs as a default lifelong solution is a form of abuse, carrying significant long-term risks. A quick caution: Never stop medications abruptly based on general advice. Only discontinue when your blood pressure normalizes naturally. Rash decisions can be dangerous.
We traditionally view normal blood pressure as 120/80 mmHg. Readings between 120-140 systolic signal pre-hypertension, a warning phase, while over 140/90 confirms hypertension. However, in 2017, U.S. guidelines shifted: normal is now under 130/80, with 130+ as stage 1 and 140+ as stage 2. Europe and Korea haven't adopted this, and even some American primary care doctors resist it. Who decides these thresholds? Cardiology societies and committees. But why the constant adjustments? Modern medicine targets symptoms, suppressing those that are uncomfortable or life-threatening. Hypertension's danger lies in its silence—its "first symptom" might be a fatal heart attack or stroke, with half such events ending in death. This prompted preventive drug development. Unlike painkillers, demanded due to immediate suffering, hypertension drugs emerged from scientific discovery: unchecked high pressure leads to sudden cardiovascular catastrophes. Yet, this insight came from an era of limited physiological knowledge—akin to Stone Age medicine. Today, we recognize the approach as overly simplistic: focusing solely on lowering pressure ignores the bigger picture. It's like glimpsing one puzzle corner and claiming to see the whole. Despite decades of aiming for under 140/90 with drugs, outcomes haven't improved—strokes, acid reflux, and dementia continue to rise. Pharmaceutical innovation has yielded varied meds: calcium channel blockers to relax vessels, ACE inhibitors to block constricting enzymes, alpha/beta blockers to dull nerve signals, and diuretics to reduce fluid volume. These curb the heart's force, which helps short-term but harms over years or decades. Heart attack and stroke statistics remain stagnant, begging the question: Why persist? The industry, heavily influenced by pharmaceutical giants, can't easily abandon established paradigms. Instead of rethinking, they targeted cholesterol next, adding statins despite evidence that vessel blockages, not just pressure, are key. New treatments require patentable drugs for acceptance; alternative approaches are sidelined. With no further breakthroughs, guidelines tightened to 130/80, conveniently boosting sales. Is there proof that 140-160 systolic severely damages vessels? Not definitively. At 150/95, we note it's high, but harm isn't guaranteed. Still, don't dismiss readings in the 120-140 range—they signal underlying issues needing attention, even if pressure alone isn't destructive. True emergencies hit at 180/120+—hypertensive crisis. Seek immediate care; in the U.S., doctors often call emergencies. In places like Korea, high costs deter visits, but ignoring advice risks catastrophe and potential lawsuits. Meds buy time here, but prioritize root-cause fixes. Prolonged highs inflame vessel walls, build plaque, and thicken the heart's left ventricle (hypertrophy), reducing efficiency and risking failure, kidney damage, or blindness. This overlaps dangerously with diabetes, as both assault fragile capillaries.

Conventional medicine labels most hypertension "essential," meaning cause unknown. Why? They seek a single, provable culprit, ignoring interconnected factors—like a courtroom acquitting suspects without airtight evidence. Think of infamous unsolved cases, like the JonBenét Ramsey murder: abundant clues, but no conviction without a body. Suspects in hypertension? Often insulin resistance from metabolic syndrome, fueled by excessive carbs, stress, or nutrient deficiencies. To grasp this, understand blood pressure's purpose: it's the heart's force against resistance to circulate blood, delivering oxygen, nutrients, and immune cells while defying gravity. Systolic (higher number) occurs during heart contraction; diastolic (lower) during relaxation. Normal 120/80 ensures brain perfusion (systolic) and sustained vessel pressure against gravity (diastolic). It's not fixed—rises with demands like exercise (up to 220 systolic is normal). Hypertension means it stays elevated, unregulated. Compensatory rises occur when delivery falters: smoking introduces carbon monoxide, slashing oxygen capacity by 20%; anemia limits hemoglobin; tall statures demand more pressure (e.g., 140/92 as baseline). Stress is the biggest driver—not just mental, but any bodily demand for more effort. Positive (exercise) or negative (traffic, work woes, finances), it tenses vessels, elevating pressure. "White coat syndrome" exemplifies this: clinic anxiety spikes readings by 20-30 points, a recognized phenomenon. Chronic stress elevates cortisol, spiking blood sugar and insulin, fostering resistance—leading to weight gain, diabetes, and higher pressure. Malnutrition, like low vitamin C or protein, weakens vessel walls, reducing elasticity.

High blood pressure isn't random misfortune; it's often a signal of imbalance. In future discussions, we'll cover practical lifestyle guidelines—what truly helps, what's insufficient, and what's risky. For now, explore related resources on diabetes and cholesterol management. Remember, shift your focus from merely treating disease to cultivating wellness. Share this knowledge, and stay informed for a healthier life. Dr. Cho is dedicated to providing evidence-based insights to help you reclaim your health.
