
Hello, everyone. This is Dr. Jo. In our previous episode, we explored the various causes of hypertension. Understanding these causes is crucial because it empowers patients to make changes that could potentially normalize their blood pressure without solely relying on medication. While medications play a key role in controlling blood pressure today, they come with significant costs and side effects. It's not impossible to manage without them, which is why reflecting on questions like "What did I do wrong? What went awry to cause my blood pressure to rise?" is so important.

In modern medicine, essential hypertension is often described as having no identifiable cause—it's just "how it is." However, from a functional medicine and human physiology perspective, we discussed several plausible factors in the last broadcast. High blood pressure is indeed dangerous. Some people reject conventional medicine and decide against taking blood pressure medications without any alternative plan, which is risky. They dislike meds, avoid other blood pressure-lowering strategies, and simply let their hypertension go unchecked. I must emphasize at the outset: this is extremely hazardous.
High blood pressure increases the risk of other vascular diseases, such as kidney problems, eye issues, and damage to capillaries. It also elevates the overall risk of death. Conversely, low blood pressure means that peripheral tissues and organs don't receive adequate oxygen and nutrients, leading to impaired bodily functions. For instance, the brain might suffer, resulting in memory loss, dementia, or even stroke. The heart needs proper blood supply to function healthily and pump effectively. If low blood pressure deprives it of resources, the heart could fail. Paradoxically, the heart might overwork to compensate, raising the risk of heart attack or myocardial infarction.
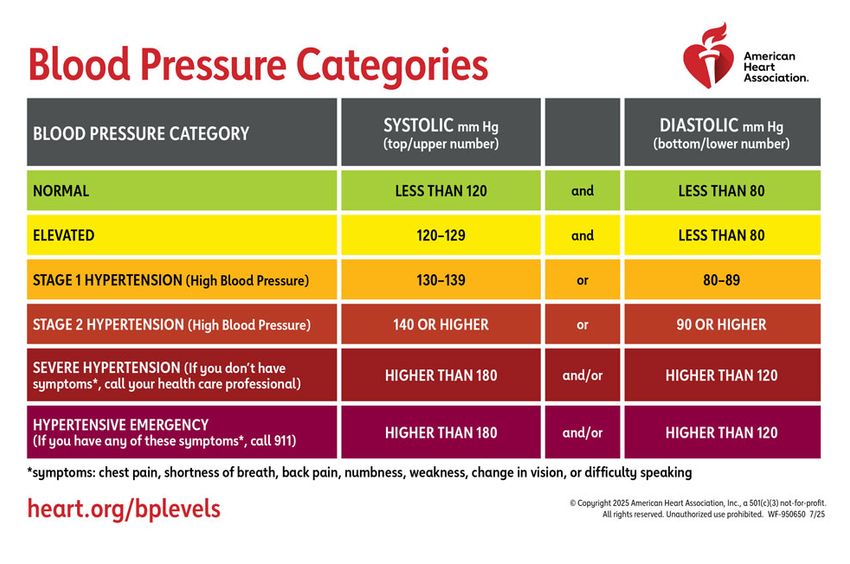
When we take blood pressure medications, we're artificially lowering blood pressure, but for some patients, this "normal" level might actually be hypotension. Remember, the nervous system, heart, and blood vessels don't raise blood pressure arbitrarily. They do so because, without it, cells in remote parts of the body won't get the oxygen and nutrients they need. Medications force blood pressure down to what modern medicine deems "normal" (e.g., 120/80 mmHg), but this ignores individual factors like age, height, muscle mass, weather, or season. The universal "normal" blood pressure standard is meaningless and could result in a state that's hypotensive for that person.
As a patient, this induced low blood pressure can lead to the very risks we mentioned—stroke or heart failure—which are the primary dangers for hypertensive patients. That's why we prescribe meds in the first place: to prevent those outcomes. But if lowering blood pressure artificially creates the same threats, it becomes confusing. You might think, "So, should I take the meds or not?" Approaching it that way leads to no clear answer. This topic is complex and can't be boiled down to a five-minute soundbite. Don't blame me for raising these thorny issues; reflect on why you haven't pondered them before.
Today, as promised, we'll review lifestyle guidelines for hypertension patients or those aiming to prevent it. The list on your screen comes from hypertension societies: nine lifestyle rules to prevent or manage high blood pressure. These are similar to the Mayo Clinic's (in the U.S., not Japan) 10 commandments for hypertension management. Some are excellent advice, but they often lack explanations of *why* they work. Others are ineffective because the underlying mechanisms aren't understood. Let's break them down one by one.
This is common advice, and it's not wrong. Excess weight requires more blood vessels, increases physical resistance, and necessitates higher blood pressure to circulate blood effectively. So, weight loss is beneficial. However, abdominal fat is often a *result* rather than the cause—stemming from insulin resistance, which also contributes to diabetes and hypertension.

Telling diabetic or hypertensive patients to "just lose weight" misses the point. If they successfully lose weight by addressing root issues, blood sugar, blood pressure, and cholesterol improve not because of the weight loss alone, but because the body normalizes overall. Insulin resistance is key here. Blaming belly fat is like scolding a symptom: "Why is my blood pressure high? It's your fault!" Belly fat would protest, "I'm the victim too!" It's a walking indicator of health issues, visible without blood tests or scans.
Focus on real changes: eat whole foods intermittently, avoid processed foods and artificial sugars, and increase healthy fats to stay satiated. This naturally lowers insulin, making weight maintenance impossible—fat melts away. Weight and blood pressure improve together, but losing weight alone doesn't automatically fix blood pressure.
This is solid advice. But why? Exercise temporarily spikes blood pressure (even to 200+ mmHg), which seems counterintuitive. The mechanism: Exercise is the ultimate brain stimulator. It engages sensory nerves (sight, touch, sound, taste), motor nerves (for movement and balance), and autonomic nerves (heart rate, breathing).

The brain regulates blood pressure—directing the heart and vessels. We receive 90% of brain stimulation through movement. Exercise activates the frontal lobe, which suppresses stress (a driver of high blood sugar and pressure). During exercise, sympathetic nerves raise blood pressure as needed. Post-exercise, parasympathetic nerves dominate, lowering it overall. Thus, exercise indirectly reduces blood pressure by balancing the nervous system.
Excellent tip, but with caveats. Fruits in excess or juiced can spike blood sugar (e.g., blended strawberries have a higher glycemic index than whole ones), worsening insulin resistance. Focus on whole forms.
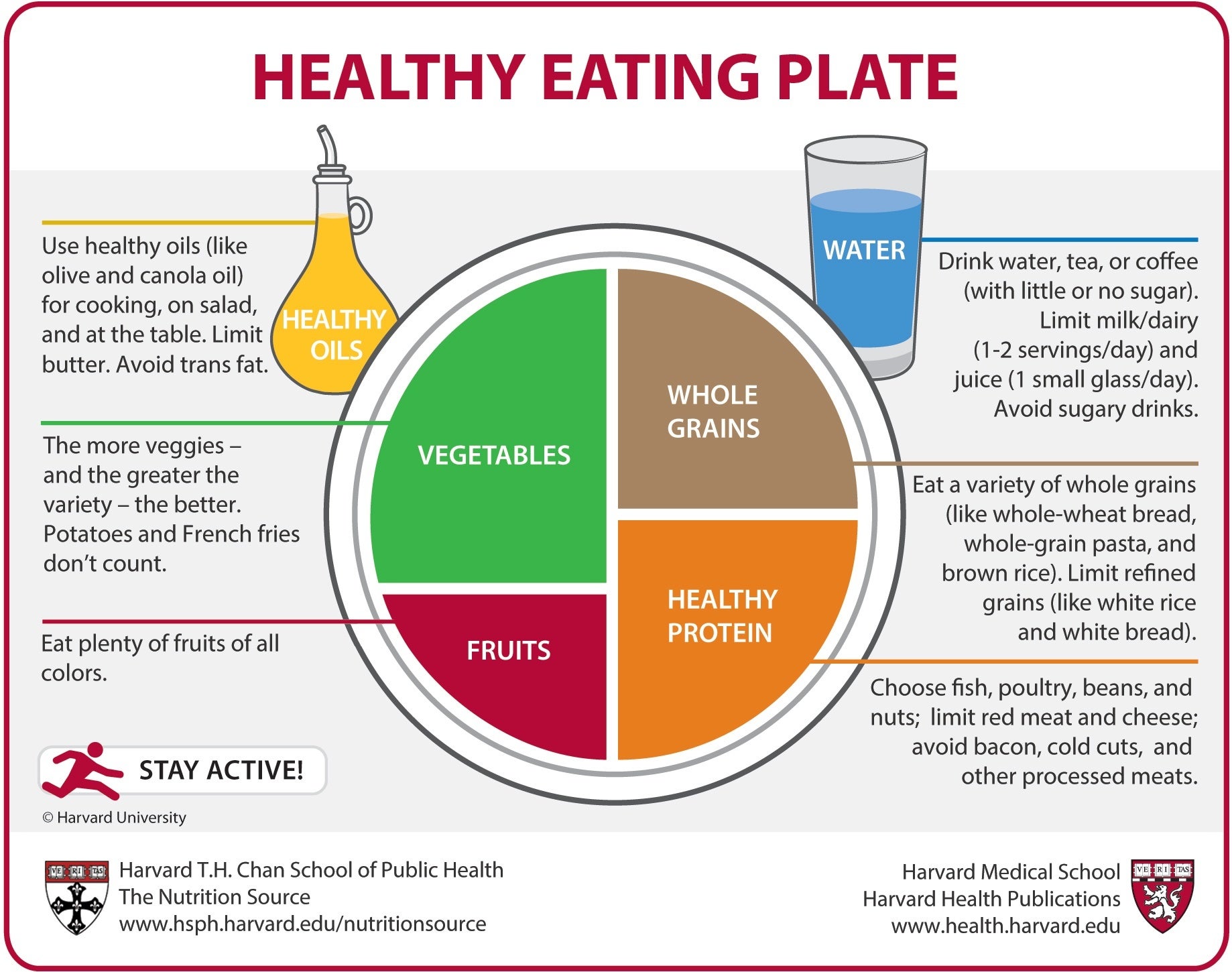
This targets insulin resistance. Sugary foods are obvious culprits. Fatty foods are flagged because saturated fats are thought to clog vessels and raise cholesterol and pressure. But dietary fats don't cause weight gain or vessel blockage. Egg yolks' cholesterol doesn't directly plaque arteries. Inflammation from carbs and sugars drives high cholesterol; fats are the least inflammatory macronutrient and least insulin-spiking.
Low-carb, high-fat diets (LCHF) are therapeutic, healing gut inflammation. One regret: these guidelines should emphasize portion control or intermittent fasting (e.g., eating twice a day). Korean guidelines improve on Mayo's by not pushing carb-heavy diets. Mayo's "healthy diet" echoes the failed Harvard food pyramid: 60% carbs, leading to epidemics of diabetes and hypertension over 40 years. Pre-diabetes often progresses to diabetes because such diets are ignored.
This is controversial—the highlight today. Salt attracts water via osmosis, increasing blood volume and pressure. True, but it ignores natriuresis: When pressure rises slightly, kidneys excrete massive water and salt to normalize it. The body maintains homeostasis (constant temperature, pH, blood pressure, sugar).

Why doesn't exercise (spiking pressure to 220 mmHg) trigger frequent urination? Because high pressure is needed for survival then—the system overrides natriuresis. Sweat helps too. The brain orchestrates this: Sympathetic dominance during stress/exercise raises pressure via angiotensin II, which prompts vasopressin (antidiuretic hormone) to retain water and constrict vessels.
Salt intake raises pressure temporarily, but homeostasis corrects it. Low-salt diets can cause sodium deficiency. Kidneys filter 250L of blood daily but excrete only 1.5L urine, reabsorbing 97% of sodium—it's precious for signaling and muscle function (heart, vessels, stomach). Low salt hinders hypertension healing; it's symptomatic control, not cure—like frequent small meals for diabetes management, not reversal.
Caution: Those with kidney failure or heart failure should limit salt to avoid complications. Most hypertensives don't fall here.
Spot-on. Moderate alcohol (1-2 drinks) may lower pressure by relaxing parasympathetics, but excess stimulates sympathetics, causing aggression and insulin resistance via liver strain. Quit or halve intake stepwise.
Smoking impairs red blood cells' oxygen transport, forcing higher pressure for delivery—quit to normalize.

Mayo suggests cutting coffee; caffeine mimics adrenaline, narrowing vessels. Temporary spikes are fine in healthy people (like exercise or salt). Problematic if adrenals are fatigued or stress is chronic.
Patients often dismiss this as cliché, but it's paramount. Untreated stress prevents fixing insulin resistance or thyroid issues. Even perfect diet/exercise fails if stress dominates. If quitting smoking or healthy eating stresses you more, don't force it—it's counterproductive.

Stress signals resource needs. Clinics say "manage it" without how-tos. Mayo: "Avoid stressful situations." Unrealistic! Stress is our reaction to events, shaped by mindset. I post on mindset in my blog/YouTube to help heal hypertension.
Techniques: Breathing exercises, movement. Counter cortisol with oxytocin (via social bonds)—details in a future episode.
Vital advice. But caveat: Ensure your doctor understands functional approaches. Many default to meds immediately, ignoring alternatives. Essential hypertension's "unknown cause" label discourages self-healing, but it's not abandonment—emergencies abound.

If on meds, don't stop abruptly; change habits first, then taper under guidance. Normal pressure on meds doesn't mean cured. Functional issues like hypertension are fixable functionally.
Choose: Restore function or manage with meds? Most want restoration. I'll share unbiased, latest functional medicine info openly. More on hypertension ahead—rewatch for insights.
Thanks for sticking through this long episode. Take care!